INTEGRATED HUMAN PRACTICES
OVERVIEW
Through human practices, we adapted our experimentation, model, and policy proposals based on the expert opinions of industry and academic professionals. To establish project need, we interviewed doctors and conducted surveys to gain a deeper understanding about the urgency of blood shortages. Our survey results from blood banks and the general public prompted our design of a mock-up user interface for a possible official blood donation app for mobile devices and the creation of our policy brief on revamping Taiwan’s healthcare point system. Furthermore, we reached out to experts in blood banks and professors to determine our experimental direction. Our human practices have played a major role in our collaboration and education initiatives from hosting a global SDG challenge and conference to collaborating with other teams where we created multiple outlets for synthetic biology promotion within our community. Human practices have informed our project direction, development, and execution in all aspects of our project.
ESTABLISHING PROJECT NEED
Prior to finalizing our project idea, we performed in depth research about how our project is needed in the industry. Our research included hosting multiple interviews with professionals within the medical field, as well as developing surveys to be distributed across communities around the world. Our team gained a better understanding of the mission and foundation of our project by conducting interviews and analyzing the distributed surveys.
Taiwan Blood Services Foundation - Mr. Jun-Hong Liu
We sought to understand how our project would fit into the current framework of blood processing facilities in Taiwan, which led to us interviewing Mr. Jun-Hong Liu (劉俊宏), the Director of Planning for the Taipei Blood Center of Taiwan Blood Services Foundation (台北捐血中心企劃課課長).
Mr. Liu believed that our project has a strong purpose and would be very helpful in tackling the blood shortage issue. He recognized that our project would benefit remote islands and cited Taiwanese islands (Green Island, Jinmen, etc.) as an example. He informed us that currently, these islands’ blood supplies are sustained by mainland blood services. However, the prolonged blood shipment process could result in immediate shortages if an accident occurs and there is a blood type incompatibility issue due to the limited blood supply in off-mainland territories.
Mr. Liu also provided input about our experimental procedures and prototype design, which is elaborated in the Experimental/Prototype Design section below.

Figure 1 - Interview with Mr. Jun-Hong Liu (upper left)
Hospital Blood Bank - Dr. Jimmy (Chun-Ming) Kang
To assess the feasibility of our project and better understand how our final product would fit into Taiwan’s existing national blood supply chain, we participated in a virtual meeting with Dr. Jimmy (Chun-Ming) Kang, a doctor at the National Taiwan University Hospital. Dr. Kang works at the hospital end of the blood supply chain to manage the blood received from the Taipei Blood Center and process the necessary units for patients.
Dr. Kang clarified that he ultimately views our project to be beneficial in ameliorating blood shortage issues, as O type blood is constantly in the highest demand. However, the blood type conversion method we are proposing would primarily be used on a need-based basis, as the blood shortage issues are periodic in Taiwan and type specific donations are still preferred due to lingering antibodies that remain in the serum of packed red blood cells (RBCs). This led us to broaden the scope of our project’s target audience by expanding to other countries outside Taiwan, leading us to create a survey for blood banks worldwide, which can be seen further down in the page. Dr. Kang further revealed that young people in Taiwan donate blood less frequently, which would become a problem for Taiwan in the future. This information led us to create a public opinion survey, a blood donation app proposal, and educational resources
aiming to increase blood donations among the younger generation.
Dr. Kang also provided us with input in regards to our blood conversion kit model, which is elaborated in the Experimental/Prototype Design section below.

Figure 2 - Interview with Dr. Jimmy Kang (third from left on top row)
Transfusion Medicine in Hospitals - Dr. Gua-Che Lu
Since our project concerns transfusion medicine, we interviewed a trauma doctor to improve our understanding of the blood transfusion process in the hospital and emergency room. We interviewed Dr. Gua-Che Lu (盧冠澈), an emergency medicine physician at the Keelung Hospital. From the interview, we learned that blood transfusions in emergency rooms are used to maintain the patient’s vital levels to allow for surgery to stop internal bleeding. If a patient needs a blood transfusion, the doctor will contact the hospital’s blood bank for the patient’s specific blood type. If an immediate blood transfusion is needed, the patient will first be given 1-2 packs of the universal O negative blood, before the patient’s blood type is tested. Then, the patient will receive the blood type specific to their true blood type. He confirmed that our project, if successful, will be applicable for both the hospital and ERs as the time from performing the extra procedure of blood type matching will be eliminated.

Figure 3 - Interview with Dr. Gua-Che Lu
Interview with Dr. Frank Hsiao
We went to the Far Eastern Memorial Hospital in New Taipei City to interview Dr. Frank Hsiao. Dr. Hsiao is a practicing oncologist who also subspecialized in hematology.
He believes that our project idea is feasible, especially during times like the COVID-19 pandemic where blood donation rates are low. He revealed that under regular circumstances, our project would be most critical in developing countries or during natural disasters. After consulting with other hematologists, he concluded that using converted blood for transfusions would not be a problem, so long as the modified blood has been approved for use by regulatory reviews.
Furthermore, he directed us to resources from the Taiwan Blood Services Foundation regarding blood supply and demand in Taiwan and gave us contacts to directors of blood banks in Taiwan. We used the data from TBSF’s webpage to model the impact of our project on blood supply as shown on the Modeling Page.
Dr. Hsiao also provided us with input in regards to our experimental procedures, which is elaborated in the Experimental/Prototype Design section below.

Figure 4 - Interview with Dr. Frank Hsiao (second from the right)
Interview with Dr. Wen-Chien Chou
Towards the end of our project development, we also interviewed Dr. Wen-Chien Chou, an experienced Hematologist at the National Taiwan University Hospital and the current Chairman of The Hematology Society of Taiwan. Dr. Chou believes that our project is worth pursuing, as it adds to scientific research on the field of blood medicine, while potentially being able to streamline logistical aspects of blood delivery in emergency remote situations.
We inquired Dr. Chou on the current blood medicine situation in Taiwan in order to have a better understanding of the current demands of the medical environment. According to Dr. Chou, chronic diseases such as leukemia, lymphoma, anemia, and emergency blood losses are situations that would require the greatest need for blood transfusions. We then proposed that our project may be useful to resolve healthcare inequities with abnormally high (38.5% and 34.5% in males and females respectively) rates of anemia in the generally more rural and poorer regions of Eastern Taiwan (Chang, et al., 2016).
We also discussed factors that would cause blood shortages. Based on previous literature, we had concluded that there are strong seasonal fluctuations in blood supply. Specifically, we have observed that winter months are more susceptible to blood shortages as the cold weather leads to fewer people being willing to leave their homes to donate (American Red Cross, 2019) while more people experience a myriad of medical conditions such as acute gastrointestinal bleeding (Stermer, et al., 1995). While Dr. Chou acknowledges that a drop in donation rates due to cold weather is likely, he believes that increased incidences in conditions such as gastrointestinal bleeding would not substantially increase the demand for blood transfusions, and instead, he states that the need for blood transfusion should stay roughly the same throughout the year. This became an important basis when developing our supply and demand modeling.

Figure 5 - Interview with Dr. Chou
Interview with Legislator Ching-Cheng Chuang and Professor George Chen Chuang/Chen
To contextualize our project on a policy level, we interviewed Legislator Ching-Cheng Chuang (莊敬程), a member of the Social Welfare and Environmental Hygiene Committee of the Legislative Yuan in Taiwan, and his advisor Professor George Chen (陳榮治), who are both associate professors of Biomedical Engineering in National Yang Ming Chiao Tung University in Taichung, Taiwan. Legislator Chuang has also organized blood drives in collaboration with TBSF in his constituency in Taichung, Taiwan. Regarding our project, Legislator Chuang and Professor Chen emphasized the need to firmly clarify when enzymatic cleavage would be needed. Legislator Chuang stated that the most effective way to mitigate blood shortages would be to increase the supply of blood. Despite this, he still sees great practical potential in the application of our projects. Specifically, he suggested that rather than waiting for a shortage situation, we could universally and permanently apply the system within the blood logistical process. Such universal cleavage would make all donated blood O type universal blood, which can save medical and blood bank personnel valuable time to get the blood into the patients’ bodies.
Legislator Chuang and Professor Chen also provided input about our prototype design, which is elaborated in the Experimental/Prototype Design section below.
Public Opinion Survey

Figure 6 - Image of the Public Opinion Survey

Figure 7 - Correlation Between Blood Type and Weighted Average of Willingness to Donate on a Scale From 1-5

Figure 8 - Willingness to Accept Modified Blood Modified
Through a public survey, we engaged with many people around the world to assess the public’s donation tendencies, understanding, and stance on bioethics of blood donation. First, we asked whether the individual has donated blood before and whether they are willing to donate blood. We asked other demographic questions, such as blood type, job, age, etc. to see if they affect their willingness to donate. Based on our results, people of AB blood type express the most willingness to donate (Fig 7), yet AB blood tends to be the lowest in demand (NHS Blood Donation, n.d.). Therefore, we believe that our project would help mitigate blood shortages since AB donors’ blood can be converted with our enzymes to O type that is in the highest demand(Red Cross Blood Services, n.d.). Then, we asked which factors deter and encourage them to donate blood, leading to our question about how willing they were to receive the genetically modified blood our project aims to create. From our survey, we concluded that assuming equivalent and safe conversion to O-type blood after our modification, most respondents would be willing to receive such a transfusion. (Fig 8) This suggests that our project would be beneficial, seeing that we are unlikely to encounter bioethical issues upon transfusion with converted blood. Moreover, our survey results support that such a biotechnological advance involving human-modification from “natural blood” is not a significant deterrent to one’s willingness to receive blood converted by our prototype. We promoted our survey through the iGEM General Slack channel, individually messaging iGEM teams on our team's Instagram account, and reaching out to our family and friends requesting they continue spreading our survey. Overall, we received a grand total of 1,520 responses from individuals across 31 countries. Our public opinion survey helped us solidify our marketing, promotion, and policy aspects of our project.
Blood Bank Survey

Figure 9 - Image of Blood Bank Survey
To help our team develop a practical and useful procedure for our project, we decided to survey blood banks around the world. This survey contained more technical and experimental questions such as whether these organizations believed that the conversion of blood types to the universal donor blood type O would alleviate the blood shortage problem. Additionally, we asked for the ideal process of converting the blood types to O; this includes the ideal time for the entire process and their preference for a hands on or hands off procedure. We reached out to eighty blood banks in Taiwan, Europe, and North America to help take our survey to give us more insight. We were excited to receive a response from the Australian Red Cross Lifeblood organization, which is described below.
Australian Blood Bank Meeting
Australian Lifeblood reported that our project would be very useful in alleviating potential blood shortage issues in their blood bank, especially on an as-needed basis. They also mentioned that in order to not disrupt the blood supply chain, the conversion process should be hands-off (automated) and can take up to a maximum of 1 hour. Ultimately, their priorities during the conversion process is efficiency, manpower, and cost, in descending order of importance.
Australian Lifeblood showed strong interest in our project and emailed us requesting a virtual meeting to learn more about our conversion process. We conducted two meetings with them, where the first was with our PI’s, and the second was with representatives from our Human Practices, Experimental, and Modelling teams.
We met with David Irving (Research Director), Alison Gould (Scientific Communications Specialist), and Rebecca Griffiths (Senior Research Fellow, specifically for Product Safety) through a Google Meeting. They presented an overview of their organization, which coordinates blood collection and dissemination across all of Australia. Annually, they receive approximately 1.5 million blood donations and oversee 80 blood donation sites and four major processing centers across the country.
However, most of the blood processing centers, donation sites, and hospitals are located in coastal cities in Australia. As such, rural regions in central Australia are more difficult to access, so in cases of emergency, air transport is utilized to deliver blood supply. They stated that in regions like central Australia and in military or emergency situations, our project would be an incredibly helpful application.
Australian Lifeblood also provided input about our prototype design, which is elaborated in the Experimental/Prototype Design section below.
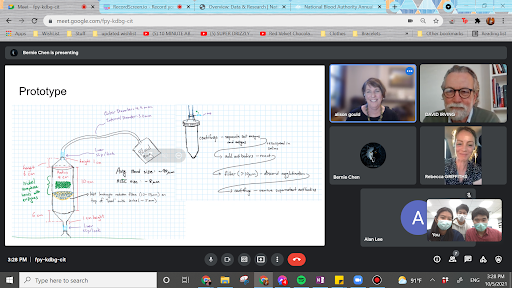
Figure 10 - Interview with Australian Red Cross Lifeblood
EXPERIMENTAL/PROTOTYPE DESIGN
To develop an efficient prototype for our project, we reached out to potential users such as researchers and medical personnels to inquire about the ideal function and design for the prototype. We found the information about the suggested total volume for one single conversion process along with the suggested filtration methods especially valuable.
Enzyme Functional Tests
Interview with Dr. Todd Lowary
Our team traveled to the Department of Biological Chemistry at Academia Sinica in Taiwan and interviewed Dr. Todd Lowary, a professor from the University of Alberta who is affiliated with Academia Sinica as a researcher. Dr. Lowary specializes in synthetic organic chemistry research with an emphasis on carbohydrate chemistry.
After the interview, we not only reflected on our experimental methods, but also connected with other researchers. On top of that, we gained access to critical materials and instruments for our project. Dr. Lowary believed that our experiments using Benedict’s Test were not optimal to test enzyme function. He generously offered A and B antigen trisaccharides for us to test enzyme function using Mass Spectrometry and Nuclear Magnetic Resonance (NMR). During the interview, we deepened our knowledge about the subtypes of blood groups, which differ based on structural differences. Our team then came to the conclusion that subtypes would not be of concern for our project as the subtypes do not substantially affect the function of our enzymes. Furthermore, Dr. Lowary referred our team to Dr. Lori West, a physician who has performed research on ABO Incompatible transplants, as we were interested in learning about the application of our project to organ transplants.
Overall, Dr. Lowary’s knowledge and input allowed us to alter our experimental procedures to test enzyme function in our own lab by using a colorimetric substrate assay. His generosity led a small group of our team to his lab at Academia Sinica to verify enzyme function using Mass Spectrometry and NMR, which is explained with more detail in the Experimental page.

Figure 11 - Interview with Dr. Todd Lowary
Interview with Dr. Frank Hsiao
During our interview with Dr. Frank Hsiao, a hematologist mentioned above in the “Establishing Project Need” section, we discussed the details of our project, specifically what we should look out for to ensure that our product would be 100% safe. Dr. Hsiao cited concerns about possible antibodies developing and reacting with miscellaneous antigens in the bloodstream. As such, we modified our prototype to include a centrifugation step where the supernatant will collect fallen antigens to be discarded and for safe isolation of fully-cleaved RBCs. Moreover, our prototype includes an additional filtration column so that any RBCs with uncleaved antigens will be trapped after being treated by antibodies in solution. These steps in our prototype ensure the complete filtration of converted blood, as just one tiny drop of incompatible blood would cause blood clotting or severe hemolysis to occur in the bloodstream, which could result in the patient’s death.
As a practicing medical doctor, Dr. Hsiao also provided helpful insight on how our project could be improved in the eyes of a doctor. He emphasized that the life expectancy of our converted red blood cells should be sustainable for the patient, which guided us to design a Percent Hemolysis experiment to determine whether enzymatic conversion of RBCs increases cell lysis.
Blood Type Conversion Kit Prototype
Interview with Taiwan Blood Services Foundation Mr. Jun-Hong Liu
In addition to his help establishing our project needs, Mr. Liu also informed us of current Taiwanese blood bank processes for blood treatment and storage. He believed that assuming our project is successful, our conversion process would occur before storage in the blood supply chain because only then can type-specific excesses and shortages be identified. He envisioned our enzymatic conversion process to proceed after centrifugation where RBCs have been separated from blood serum.
Mr. Liu also stated that he viewed mechanizing the blood type conversion process as an integral aspect to consider for our project implementation due to the volume of blood being processed daily (~2200 bags) and the number of personnel overseeing processing (~40 people). As such, we began considering our prototype’s compatibility with mechanization for improved efficiency and designed the first half of the conversion process to be mechanized. Furthermore, he elaborated on safety regulations that must be enforced, specifically noting the importance of airtight transfer and temperature control. To address Mr. Liu’s concern of airtight transfer, we designed our prototype to have Luer-Lock style connectors which are commonly used in the health industry. With regards to temperature, Mr. Liu warned that blood leaving cold storage conditions (>1°C - 6°C) for more than 30 minutes will cause RBCs to deteriorate. After receiving Mr. Liu’s input, we realized two feasible possibilities: the first would be for our prototype to be used in 1°C - 6°C storage conditions, and the second would be to pair our prototype with temperature controlled machinery. This further inspired us to do Q10 experiments on our enzymes to determine the temperatures at which our enzymes can function efficiently.
Ultimately, the question of whether our prototype can be implemented into Taiwan’s existing blood processing framework lies in cost benefit analyses. We would need to consider the cost required for our prototype to function, including enzyme and antibody costs, as well as the amount of unconverted RBCs lost through transferring blood through each vessel in our enzymatic conversion prototype. Optimizing the amount of blood converted versus blood lost is critical if our project were to be applied generally. However, if we choose to present our project as a solution for need-based crises in more remote settings, his concerns can be considered to a lesser degree. We addressed his concerns about cost by developing a marketing plan, which can be seen here.
Interview with Dr. Jimmy Kang
In our interview with Dr. Jimmy Kang, a doctor who works at a hospital blood bank mentioned above, further gave input on our blood conversion kit prototype. Dr. Kang advised that for each blood conversion procedure, it would be best to convert one unit of blood at a time, which is around 250 mL in Taiwan; the units may differ between countries. Additionally, he mentioned that a hands on, uncomplicated, disposable blood conversion process is sufficient as machinery may be expensive and may have possible errors that still need to be corrected by manpower. Thus, we designed the second half of our prototype conversion process to be hands-on. Dr. Kang highlighted the importance of optimizing our project from a cost benefit standpoint, as the higher the temperature above 4 °C, the more RBCs are lysed; however, lowering temperature also decreases enzyme functionality. We accounted for concerns he raised as we designed our prototype as integrated human practices.
Interview with Legislator Ching-Cheng Chuang and Professor George Chen
In our interview with Legislator Ching-Cheng Chuang (莊敬程), and his advisor Professor George Chen (陳榮治), we proposed our original prototype idea of etching our enzymes to small nickel sepharose beads, 90 μm in diameter, and placing it in our prototype for the cleavage reactions to occur. The beads are identical to the beads used in the protein purification process, and by transplanting those directly to the prototype, we can cut down on the complexity and the number of steps required to manufacture our prototype. With this method, we would not need to remove then reattach enzymes to another surface on our prototype.
However, Legislator Chuang and Professor Chen expressed concerns about the bead placement in our prototype. Considering that the blood product will ultimately be transfused within the human body, there may be risks that beads may fall off and ultimately be transfused into the body, causing adverse health effects. As an alternative, they suggested using a porous filter at the bottom of our columns, made out of hydroxyapatite, a biocompatible material commonly used to make toothpaste, then etching our enzymes onto the material. Such a filter would resemble bacterial pebbles in a fish tank or high porosity road pavements.
Legislator Chuang and Professor Chen also suggested that if we are to use beads, we should use Platinum or Gold beads, as they could have lower reactivity rates compared to other materials. After literature research, we learned that nickel metal and nickel compounds could harm red blood cell function, specifically through impairing hemoglobin reactivity. (De Luca, et al., 2007), (Tkeshelashvili, et al., 1989)
Given these concerns, we decided to improve upon our prototype to address the issues raised. Our own research suggests that hydroxyapatite (and similar materials) may induce the aggregation of red blood cells, sticking to them and ultimately damaging the cells. (Han et al., 2012) Therefore, weighing these options, we decided to continue using the beads system, adding a plastic leukocyte filter, with small porous openings between 10-50 μL, allowing red blood cells to move through while at the same time blocking beads from moving through. We also were concerned about the use of Nickel sepharose beads. However, after the interview, we determined that since the amount of Nickel material would be relatively small (given that our beads are quite small), and thus would not make a significant impact towards red blood cell function.

Figure 12 - Interview with Legislator Ching-Cheng Chuang (top left) and Professor George Chen (top right)
Interview With Australian Lifeblood
In our interview with David Irving (Research Director), Alison Gould (Scientific Communications Specialist), and Rebecca Griffiths (Senior Research Fellow, specifically for Product Safety), they raised the concern that the enzymes immobilized on nickel seraphose beads may fall off during the conversion process, potentially causing adverse reactions in the converted blood. They also suggested that we consider replacing our centrifugation processes with an additional column filtration step instead if our conversion system were to be used in emergency settings. Moreover, they voiced their concern about the increased cost due to the nickel sepharose beads, but as our current prototype is meant to be single-use, cost and increased plastic usage decreases feasibility.
They suggested that we continue researching methods to immobilize our enzymes on various membranes, paying particular attention to the chemical composition of the membranes. For instance, they proposed lateral flow units, leukocyte dilution filters, and gravimetric flow columns, which simultaneously separate red blood cells and the rest of the whole blood while cleaving blood antigens. However, we ultimately decided that gravimetric flow columns are unfeasible because the conversion process would take too much time.
PROJECT EXECUTION
We proceeded to not only promote but also attempt to integrate our project into our community by proposing governmental policies and creating a blood donation app. In addition to integrating our project into our community, we had students from our team travel to blood donation sites to experience the blood donation process.
Policy Proposals
Despite Taiwan boasting an affordable and advanced healthcare system for its citizens and having the highest blood donation rates in the world, it still experiences irregular shortages in blood. Therefore, we sought out to explore a myriad of different policy change proposals in Taiwan, whether for private blood collection organizations or governmental regulations, with the goal to further mitigate blood shortages through different reforms.
Blood Donation App
We pitched our proposal for Taiwan Blood Services Foundation (TBSF) to create an official blood donation application (app) by explaining the rationale for why we view there to be a need for this app and presented the mock-up user interfaces (UIs) we created. The purpose of such an app would be to create a centralized, simplified, yet cohesive source of information optimized for mobile devices. We stated that the app would incentivize regular donors to donate consistently and encourage new donors to learn more about the blood donation process and its merits. Additionally, due to its compatibility with mobile devices, the app aims to target a younger, mobile device using demographics who have been statistically shown to donate less. In general, consolidating information related to blood donation in an app format enhances users’ ease of access as users can now obtain pertinent information on the go.
Within the app, blood shortage updates and alert notifications are provided in conjunction with relevant news, stories, testimonials, and reports. To make blood donation appointments, an interactive scheduling calendar paired with live donation site updates in google maps is set up for ease of access and easy booking. A “contact us” feature is also available for direct contact with TBSF when support or enquiries are needed. Additionally, the app provides a shop page to exchange prizes with donation points given after regular blood donations. Mini-games are also available to enhance user knowledge on blood donation practices and statistics. Moreover, infographics, animations, and short videos within the app will be more user-friendly and comprehensible compared to the current TBSF website. Language options are also accessible for user language preferences. Finally, a complete FAQ (frequently asked questions) section offers users information regarding eligibility, scheduling, pre-donation and post-donation guidelines, donation and sanitation processes, and many more. Users can utilize all in-app functions after logging in to their eDonor account, which stores needed user information such as personal health statistics and donation history. However, Mr. Jun-Hong Liu, the director of planning for Taipei Blood Center, cited liability concerns to the app due to fears of personal information being prone to leakage when moving to mobile phone app format, thus TBSF would not be able to bring the app to real life despite its numerous benefits.

Figure 13 - A few of our Blood Donation App mockup user interfaces
Healthcare Spending Policy
We interviewed Legislator Ching-Cheng Chuang (莊敬程), a member of the Social Welfare and Environmental Hygiene Committee of the Legislative Yuan in Taiwan, and his advisor Professor George Chen (陳榮治), who are associate professors of Biomedical Engineering in National Yang Ming Chiao Tung University in Taichung, Taiwan. Being familiar with the Healthcare system here in Taiwan, Legislator Chuang and Professor Chen offered valuable insights to our fiscal policy proposals that are to make the implementation of our project financially viable. As he explained, Taiwan is under a single payer system managed by a governmental agency, with the National Health Insurance (NHI) program awarding a predetermined amount of NHI points - shares of the total annual healthcare expenditure - to hospitals and other organizations for every medical procedure covered by the program. This is known as an ‘Expenditure cap' system, and is used to cap the amount of healthcare spending each year (衛生福利部中央健康保險署, 2005). Each point is now worth around 0.92 NTD (roughly 3.2 US cents)(Chen, 2020).
As it currently stands, NHI awards 575 points to blood banks for every whole blood bag processed (Chen, 2017). Thus, we proposed raising the amount of points (upwards to 900 points) awarded to cover any additional costs for the implementation of our blood antigen cleavage system, such as column costs, enzyme costs, and extra costs in labor and handling of the blood product. Yet, throughout the years TBSF (the only blood bank organization in Taiwan) has consistently earned a net asset (having higher revenues from existing NHI funding than expenditures in organizing blood donations), building up a considerable cash reserve (Taiwan Blood Services Foundation, 2019). Because the point system constitutes shares of a limited pie, healthcare funding is a zero sum game; unnecessary increases of point award in the handling of donated blood would take away valuable funding in other sectors of healthcare (such as eldercare and emergency medicine). Therefore, Legislator Chuang suggests that TBSF should be financially responsible for increased costs in blood antigen cleavage, as they could most likely afford so without increases in governmental assistance.
Relaxation of Blood Donor Restrictions
We interviewed Dr. Wen-Chien Chou, an experienced Hematologist at the National Taiwan University Hospital and the current Chairman of The Hematology Society of Taiwan. Dr. Chou notes that to increase the amount of donations, adjustments in eligibility policy to increase the donor pool. Currently, Taiwan has strict rules in regards to who can donate and who cannot. In particular, those who are above age 70 (with considerable restrictions after age 65) and/or those who have high blood pressure are strictly prohibited from donating, even though many are perfectly healthy and other eligible. He argues that certain restrictions such as these could be loosened. However, he does note that blood banks put the wellbeing of donors and blood recipients first, and they are often wary of the risks that come with loosening restrictions. Any modifications to current regulations thus need to be mild to prevent any unintended negative health consequences for the donor or patient, as this would be worse than having a shortage in blood.
iGEMers Blood Donation Trips
Over the past months, several members of our team went and donated their blood, as Taiwanese law allows for those aged 17 and above to donate blood without parental consent. Below is a recount of their experiences.
Alan L. went to donate blood two times - first time in a blood donation center, and second time in a bloodmobile. Laura H. donated blood one time in a bloodmobile. Both Laura and Alan had a similar procedural experience, although the blood donation center was noticeably more spacious. After entering the blood donation site, they were asked to input personal information, medical history, and contact details on a tablet. Then, blood pressure was measured, and they reported their weights.
For Laura, another staff member asked her what she had consumed throughout the day prior to arriving at the blood donation site, and the staff member deemed the amount of food she consumed as insufficient, directing her to eat the biscuits and juice they provide outside of the blood mobile.
Next, they were directed into a small room for a brief interview, covering current medical status, sexual activity, and general physical condition on the day. A big emphasis was placed on HIV/AIDS and sexual history to prevent any adverse outcomes through blood transfusion. Both donors signed forms confirming all reported information was correct. Donors had their forefingers pricked to test blood Hemoglobin levels.
In preparation for the blood donation process, blood donation site personnel cleaned the inner elbow region of the arm with a more viable blood vessel. Donors sit on an inclined sofa-chair and a nurse begins drawing blood. As first time donors, Laura and Alan could only donate 250 mL (one unit) of blood, but in his second time, Alan was able to donate 500 mL (two units of blood). After completing the blood drawing process, donors rested on site for approximately 10 more minutes for observation and were given complimentary snacks and beverages to consume. The whole process took roughly 45 minutes from start to finish.
From Laura and Alan’s donation trips, we learned that TBSF’s operations are very methodical and efficient. As such, we conclude that TBSF’s blood processing center likely operates in a similar fashion to their blood donation sites, underscoring the importance for our project to integrate seamlessly into existing standardized processing frameworks such that our solution does not pose as a greater hindrance than help. Moreover, we understood that the blood donation process is straightforward and optimized for donors’ comfort/safety. Knowing this, we felt more legitimized promoting blood donation to members of our community. Our promotion efforts for blood donation has been through our social media pages, roundtable discussion, and blood donation app proposal.

Figure 14 - Laura’s Blood Donation Trip in Bloodmobile

Figure 15 - Alan’s Blood Donation Trip in Bloodmobile - Image of Interview Room at Blood Donation Center
Entrepreneurship
Introduction
We envision developing a commercially viable product that will be implemented into worldwide healthcare systems to alleviate blood shortage issues. To help with this, we have conducted integrated human practices research and outreach to help guide us through the entrepreneurship aspects of our project, which includes the creation of a marketing plan and pitching our idea to world famous venture capitalists.
Blood Conversion Kit
To bring our project to life, we devised a two-step blood type conversion kit to 1) mediate the enzymatic conversion process, and 2) purify converted RBCs in preparation for transfusion. We plan to pass washed RBCs through a series of airtight columns with bead-immobilized enzymes, where enzymatic conversion will take place. Then, we will isolate cleaved RBCs through centrifugation and filtration with leukodepletion filters.
Our modeling team developed a prototype for this kit, and the theory and design of it can be found in the modeling hardware page. The experiments done to help with the design can be found here in the proof of concepts page. The prototype contains a two-step process: enzymes will first be used to cleave off antigens on RBCs, and antibodies will then be used to confirm for full cleavage of the cells.
Consulting Marketing Experts
We worked with Ms. Maggie Hsieh, VP Sales & Marketing at ACHB Enterprise Co Ltd (穎佳企業股份有限公司), along with her medical device engineering team at ACHB before we started writing our marketing plan for our product to discuss the key components of a successful marketing plan. ACHB helps to create medical devices, life science instruments, and other health related IoT devices and has an in-house regulatory analyst team to make sure that safety regulations and quality standards are met.

Figure 16 - Virtual Meeting with ACHB
In this meeting, ACHB gave us a lot of advice for if we were to set up a real company. We gained more insight into the differences in marketing in different countries. We also learned the importance of defining a target audience and outlining the value proposition. With this knowledge, we were able to better understand how to approach our marketing plan.
Marketing Plan
Though our project’s blood conversion kit is still in its prototype stage, we wanted to see how it can be used on the current market. Thus, we developed a marketing plan which can be accessed here.
In our Marketing Plan, we expressed the need for our project’s blood converting device and the lack thereof of a similar medical device on the market. We compared UniversO’s processed and converted blood to other types of blood used in blood transfusions, such as regular blood, artificial blood, as well as converted blood, all of which are defined in our marketing plan. Because of our device’s easy integration into the processing of blood for transfusions, efficiency in converting blood types, as well as the need for such a product, we believe that our device will be competitive in the market.
Our target market for our blood conversion product is the United States. The United States has recently declared a nationwide blood shortage, creating a need for our blood conversion device.
The U.S. Food and Drug Administration’s Center of Devices and Radiological Health is in charge of approving and regulating many medical devices in the United States. The availability of resources to approve our blood conversion device will allow our product to be applied in medical settings.
We decided to price our UniversO blood conversion kit at $250USD. We discussed the reasoning for this pricing in our marketing plan.
To create our blood converting device, we plan on partnering with ACHB Enterprise Company, a medical device manufacturing company established in Taiwan, that also has bases in Japan and the US. ACHB has been successful in engineering and manufacturing life science devices. By working with a local-based company that has established divisions in the US, our team can collaborate closely with ACHB to create the most effective product to then be administered in the US.
Meet the Drapers Entrepreneur Show
Two of our members pitched our project to Tim Draper, an American venture capitalist, through the Meet the Drapers Season 5 casting call (Fig 17 & 18) which airs on the Game Show Network (GSN). Meet the Drapers is a TV program where aspiring entrepreneurs pitch their start-up ideas to the Draper family and persuade them to crowdfund their business and help them start it. Tim Draper and his casting crew really enjoyed our project pitch, and chose our project as his favorite out of all the projects presented that day. We were placed through the Semi-Finals of the show, and are still waiting to hear back from them for the Finals results. If we are placed through the finals and win, we could be awarded 1 million dollars for our project startup.

Figure 17 - Tim Draper in the Meet the Drapers casting call

Figure 18 - Our team presenting our pitch during the Meet the Drapers casting call
SUSTAINABLE DEVELOPMENT
It was important for us to consider the contributions of our project to the sustainable development of the world; therefore, we turned to the Sustainable Development Goals. We were determined to encourage sustainability within our own project and the projects of other teams, which led us to collaborations with other teams pertaining to sustainability.
Introduction
The Sustainable Development Goals (SDGs) are a set of seventeen goals that the United Nations aim to achieve by 2030 (United Nations, n.d.). These universal goals address the urgent environmental, political and economic challenges in the world to achieve a better future for all (United Nations, n.d.). Some of these goals include improving health and education, reducing inequality and poverty, spurring economic growth, and tackling climate change. A full list of all SDGs and subgoals can be found here. The United Nations calls for all countries to help tackle these goals in a global partnership.

Figure 19 - List of 17 Sustainable Development Goals (United Nations, n.d.)
Tackling the SDGs
Although there were a multitude of SDGs that our project addresses, we decided to focus on goal 3: Good Health and Well-Being, 4: Quality Education, and 17: Partnership for Goals.

Figure 20 - The three Sustainable Development Goals our project focuses on
In terms of SDG #3: Good Health and Well-Being, we decided to hone in on subgoal 3.4, which aims to reduce the mortality rate from “non-communicable diseases and promote mental health” (United Nations, n.d.). Non communicable diseases, such as cancer, diabetes, or cardiovascular diseases, include conditions that are not onset by an infection and often require lifelong treatment and care. One common treatment for these patients are transfusions of red blood cells. Because patients are unable to individually synthesize an adequate and healthy amount of red blood cells, these transfusions are lifesaving.
However, the availability of blood for transfusions is regulated by the supply and demand of safe, transfusable blood. Due to issues with patient-donor specificity and decreasing donations rates among younger populations, there is a low supply of blood for these transfusions while demand continues to rise (WHO, 2010). These issues result in the inability for patients to receive critical treatment they need to live a normal, healthy life. To reduce the amount of deaths of patients with these conditions, our project can convert the incompatible blood to the universal blood type, O, which can be given to the patient until a blood supply of their own blood type comes in. Our universal blood ensures that patients are consistently receiving successful blood transfusions that will improve their quality of life, thus tackling SDG goal 3.4.
Our project also tackles subgoal 3.6 which aims to reduce the number of deaths and injuries from road traffic accidents. We interviewed a trauma doctor to better understand our project’s role in reducing deaths from accidents. In emergency rooms, blood transfusions maintain the patient’s vital levels to allow for surgery to stop internal bleeding. If there is a need for blood transfusion, the doctor will contact the hospital’s blood bank for the patient’s specific blood type. If an immediate blood transfusion is needed, such as a road traffic accident, the patient will first be given 1-2 packs of the universal O negative blood, before the patient’s blood type is tested. Then, the patient will receive the blood type specific to their true blood type. Through converting blood to the universal blood type O, our project eliminates the extra procedure of blood type matching, which can lower the number of deaths and injuries in road traffic accidents directly addressing subgoal 3.6.
For goal 4, our project more specifically targets goal 4.5, which aims to eliminate discrimination in education. As part of our project, we developed a Synthetic Biology educational website with activity packets, instructional videos, worksheets, and a reward system. Topics included fundamental lessons on central dogma, gene expression, and gel electrophoresis. Through the internet, we hope to reach a larger audience and allow anyone around the world to have access to STEM field education. Inclusivity is a central focus of this website; our free and downloadable activity packets come in both English and Mandarin Chinese, as does our website. We are able to lower the barriers -- such as accessibility and language-- to education and allow everyone to have the resources to learn about fascinating science topics. We envision that the packets can help reduce discrimination in education as they can be distributed to groups that may not have access to as much scientific knowledge and resources, especially during times of the pandemic. We distributed the website along with lab equipment to a local Taiwanese Aboriginal school, where students do not have access to extensive STEM education. We shipped over essential lab materials and carefully guided them through foundational lab techniques in a virtual event.
Additionally, our team tackled the gender disparity in synthetic biology in our collaboration event with our school’s Girls in STEM Club and FRC team. We held a STEM Workshop, an event where we invited young female students to explore through hands-on experience in the science and technology fields. Our event promoted inclusivity and equity in these male dominated fields of study and encouraged young women to break down gender barriers in STEM. More information about our education initiatives can be found below in the Education section.

Figure 21 - Home Page of our Synthetic Biology Educational Website

Figure 22 - Virtual Lesson with Aboriginal Jianshi Jr. High Students
iGEMxSDG Challenge & Conference
Not only did we target Sustainable Development Goals through our own project, we took the sustainable development impact one step further by hosting an iGEMxSDG Impact Challenge and Conference to encourage all iGEM teams to take action on these urgent global challenges. SDGs were first introduced into the iGEM community in 2019 to spread awareness of the goals. This year, we took the furthered direct contribution towards these goals by focusing on action on top of promotion.
Because SDGs are universal goals, we not only focused on the relevance of SDGs to an individual team, but rather challenged teams to target these goals on a global level by making tasks for one another. Each teams’ tasks targeted specific subgoals for one or more SDGs. With the collaboration of completing tasks across different continents, we directly targeted SDG #17: Partnerships for the Goals. We further spread awareness of SDGs by encouraging teams to post SDGs relevant to their project on social media using a template we created and nominate other teams to participate. On September 18th, we held a virtual conference with all participating teams and discussed how we tackled the SDGs.
The first task we developed for other teams to accomplish targeted goal 4.5. We asked them to distribute our Synthetic Biology educational website to groups with limited access that can be found on our website to encourage the elimination of discrimination in education. This task was completed by iGEM Team Thessaly. One of the groups they sent our website to was Mrs. Chatzipli, a professor that teaches juveniles in the Volos Prison Facilities in Greece, who exclaimed how organized and informational our lessons were. She thought our website was a really great way to provide access to education around the world. Our second task targeted goal 3.4. We wanted other teams to put us in contact with an individual who regularly receives blood transfusions for their condition. We hope that by speaking with this individual, we can better understand the importance of transfusions and its role in preventing premature mortality.
Beyond targeting SDGs for our own project, we took the initiative to help other iGEM team’s tackle their SDGs as well. The first task we completed was for iGEM Team Calgary. Their project, Neocycle, focused on developing an innovative system for recovering rare earth elements from electronic waste. Their project targets SDG #7 Affordable and Clean Energy, as well as SDG #17 Partnerships for the Goals. The task that we completed was in response to goal #7.A: enhance international cooperation to facilitate access to clean energy research and technology by connecting the team with an electronic waste recycling facility in our region.
Thus, we contacted SDTI, Taiwan's largest electronic waste recycling institute, and provided their website and contact information to Team Calgary. In the process of searching for electronic waste recycling facilities, we learned the importance of rare earth elements in electronic products and how important it is to promote sustainable recovery of these resources which directly targets goal 7.A. The second task we undertook was for iGEM Team Saint Joseph. Team Saint Joseph project, Cellulophile, focuses on degrading the top water pollutant, paper waste, with a genetically engineered enzyme to prevent water borne issues. Their project targeted SDG #6 which ensures clean water and sanitation. Their task, to distribute their google form about the use of biotechnology, directly targets goal #6.3, as we draw attention to the need to help people reach clean water, bioremediation, etc. We promoted their survey across all our social media accounts and verbally promoted the survey to students at our school. More information about the SDG conference will be listed below.
This event linked 26 teams across 16 countries together during pandemic times, and was highly praised by both the participating teams, as well as iGEM EPIC, who reached out to us in request to join the conference. For each participating team, we uploaded all their information onto our website by creating a website tab for each team. The website, which also includes more details about the challenge, can be found here. An introduction video for the challenge created by our team can be seen below.

Figure 23 - Diagram of extensive collaboration among 26 teams showing which teams completed which teams tasks.

Figure 24 - iGEMxSDG Impact Conference

Figure 25 - Members of our team presenting conference introduction slides

Figure 26 - Members of our team presenting our 4-minute presentation
iGEM EPIC, the Entrepreneurship Program Innovation Community that supports the development of iGEMs entrepreneurial community, reached out to us and requested to join our iGEM x SDG Impact Conference. The vision of the program is to become the driving force behind hundreds of SynBio based start-ups globally to help accelerate the transition to a more sustainable bioeconomy. They were very enthusiastic about our conference as they believe that infusing the spirit of entrepreneurship into feasible SynBio projects that work towards achieving the SDGs will help build a strong and sustainable SynBio startup ecosystem. They stated that projects orientated towards SDGs are in high demand in the entrepreneurship market as the problems of SDGs are universally recognized. The Head of Asia Pacific EPIC Committee, Onkar Date, joined our conference and gave a presentation on the iGEM EPIC program as well as their vision of incorporating SDGs into it. He further listened to presentations of several iGEM teams and engaged in discussions with us.

Figure 27 - iGEM EPIC presenting at the conference

Figure 28 - iGEM X SDG Impact Challenge statistics
Participating iGEM Teams:
KCIS_NewTaipei, Korea_HS, NTU-Singapore, IISER-Tirupati_India, Saint_Joseph, RUBochum, Stony_Brook, CCU_Taiwan, SHSID, NKCU_Tainan, ASIJ_Tokyo, Moscow_City, Thessaly, Sydney_Australia, William_and_Mary, NU_Kazakhstan, Aachan, MIT_MAHE, PuiChing_Macau
Wageningen_UR, ATG X iGEM UMA, Open_Science_Global, Calgary, Tu_Darmstadt, Mingdao, TAS_Taipei
OUTREACH
As part of Integrated Human Practices, TAS_Taipei sought to expand our project goals to a larger community. TAS_Taipei approached education with a two fold focus on both providing introductory concepts to synthetic biology and project-based teaching. Our team aimed to diversify the mediums for education from conducting radio interviews to creating online activity packets in order to be inclusive of as many people as possible.
Public Awareness
Bioethics Panel Discussion
In March, we hosted a Bioethics Panel to discuss the ethical concerns revolving around our project. These discussions were conducted to gain more insight into the thoughts of our TAS school community to establish a baseline for issues that our Activities/Human Practice team would address. In our panel, we explained the importance of our project through the lens of blood transfusions, the blood shortage in Taiwan, and the dangers of blood incompatibility. We then moved on to examine three topics: correlation between blood type and personality, patient consent, and the commercialization of blood.
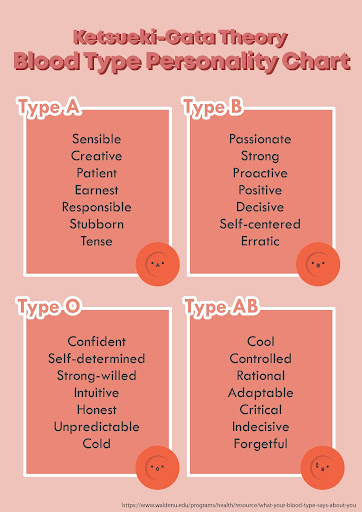
Figure 29 - Ketsueki-Gata Theory charts that were passed out during the Bioethics Panel for the Kahoot Game

Figure 30 - Roundtable Discussions

Figure 31 - Discussing the ethics of commercializing blood
To facilitate discussion among the members at each table, we played a quick Kahoot icebreaker game in which each table worked collaboratively to guess the blood types of our TAS faculty members using the Ketsueki-Gata Theory (see Fig 29). The Ketsueki-Gata Theory is embraced by many in Japanese society and is based on the notion that a person’s blood type is directly correlated to their personality. Regardless of how accurate the Ketsueki-Gata Theory is, it still offers a fun approach to thinking about the different blood types and their connection to the various personality traits (Walden University, 2021).
To test the validity of the Ketsueki-Gata Theory, we performed a Pearson’s Chi-Squared goodness of fit statistical analysis test using Kahoot results from the Bioethics Panel. We wanted to determine whether the Ketsueki-Gata Theory is an effective way to classify people’s blood types based on their personality. Our results showed that there was not a statistically significant difference between each of the blood type choices for each faculty member; essentially, each table group was merely guessing and the personality chart provided by the Ketsueki-Gata Theory was not of much assistance in the process. This shows that one cannot accurately predict a person's blood type by assessing subjective personality traits. (For further technical details, refer to CHI-SQUARED TEST FOR BIOETHICS PANEL below.
We then explored a real-life court case involving the blood transfusion performed on a member of the religious group Jehovah’s witnesses. Jehovah’s witnesses oppose receiving donated blood from others, thus opening the floor for discussion on the topic of patient consent for transfusion processes (Medical Protection, 2021).We found that the majority of attendees believed that physicians should respect their patient’s values and decisions. In regards to the discussion on the use of modified blood for transfusions, a topic that directly links to our project, we found that most participants think that the conditions of the modified blood must be outlined to the patients clearly, and should be noted down in a separate box on patient consent forms. The ideas that were expressed, including the importance of patients’ wishes and transparency between physicians and patients, were considered in our future HP works.
After wrapping up on Patient Consent, we moved on to our last topic, which was the commercialization of blood. Our attendees had different perspectives on whether blood should be considered a commodity, but when our project’s modified blood was discussed, there was a general consensus that the prices of modified blood would be based on the price to manufacture the blood. However, many attendees also believed that if modified blood were to be commercialized on a large scale, the price of modified blood would decrease. We would further explore these monetary ideas with our marketing plan.
All in all, the Bioethics Panel definitely helped us determine the ideas that we needed to further explore and address with our project.
Chi-Squared Test on the Ketsueki-Gata Theory For Bioethics Panel
To determine whether or not the blood type personality theory from the Bioethics Panel is plausible in predicting one’s blood type, we can conduct a statistical significance test to determine whether or not Kahoot participants could successfully assign the personalities of different TAS faculty members to a specific blood type after being provided with the personality chart. The Pearson’s chi-squared test determines whether there is a statistically significant difference between two sets of values, which in our case, is whether or not the distribution of votes is significantly skewed towards the correct answer choice. The formula for conducting the test is as follows:

where χ2 denotes the Pearson critical value, Oi denotes the observed value (the actual number of votes from the Kahoot for a blood type), and Ei is the expected value (each is 2.5 representing an even distribution of the 10 votes across 4 choices). Typically, the Pearson’s chi-squared test requires expected values above 5. However, Larntz (1975) found that for goodness of fit tests, a small sample size results in only minor differences, and thus we could use this chi-squared test despite our small sample size. The other statistical inference requirements had been met as well.
In statistical terms, our testing hypotheses are:
Null Hypothesis (H0): Observed # of Votes for Each Blood Type = Expected # of Votes for Each Blood Type (2.5)
Alternate Hypothesis (Ha): Observed # of Votes for Each Blood Type ≠ Expected # of Votes for Each Blood Type (2.5)
Our null hypothesis assumes that our Kahoot participants were essentially guessing, and thus the theory cannot be practically applied to determine one’s blood type. On the other hand, our alternative hypothesis assumes that the participants were able to utilize this theory to be able to predict strongly for a particular blood type regardless of whether or not the prediction is correct.
To conduct the statistical inference test, we attempted to reject the null hypothesis. This is done by calculating the χ2 critical values for each question and determining the associated P-value with 3 degrees of freedom. The P-value represents the probability of getting the observed values should the null hypothesis be correct. The lower the P-value, the more power we have to reject the null hypothesis. Conventionally, the P-value should be less than 0.05 for us to reject the null hypothesis. In our case, for the Ketsueki-Gata theory to be relevant, the null hypothesis for at least an overwhelming majority (75%) of the questions should be rejected, and there should also be a majority of answers chosen being of the correct blood type. In other words, Kahoot participants should be able to predict strongly for a particular blood type for most of the teachers and predict the correct blood type in each instance. The statistical analysis results are below.
Table 1 - Chi-squared Test results for the Ketsueki-Gata Theory

Our results show that the Ketsueki-Gata Theory of personality and blood type was not helpful for students determining the blood types of teachers as all P-values were greater than 0.05 (Table 1). The data and results from the participants were essentially equivalent to taking a random guess, as they were well distributed throughout all the answer choices. In addition, very few participants successfully matched faculty members to their correct blood type. Even though some correct answers were matched by the majority of votes, there was little statistical significance in that similarity, as they were simply the product of chance. In statistical terms, we failed to reject our null hypothesis that the observed number of votes for each choice were similar to the predicted number of votes under random chance. Therefore, the Ketsueki-Gata Theory is not effective in predicting one’s blood type, or even able to have strong predictions (even false ones) of one’s blood type over many samples.
Media Outreach
China Post
We reached out to China Post to write a public awareness article that is currently in press, discussing the urgent need for blood supply and donations in Taiwan. We first introduced our project and how we aim to develop a kit that can convert other types of blood to the universal donor O-type blood to alleviate the blood shortage issue. Then, we discussed our experience with the pandemic and how it has affected our research process. We explained the creative ways we had to come up with in order to work around the stringent COVID-19 regulations. We further explained our experimental progress and the other aspects we worked on during Taiwan’s period of lockdown. To conclude, we emphasized our project goal of spreading awareness regarding the importance of blood donations.

Figure 32 - The China Post Logo
iCRT
We were also interviewed by the bilingual local radio station ICRT, where we shared information regarding our project and the pressing need for blood donations in Taiwan. We first gave an overview of our project and how it aims to tackle the issue of low blood supply through the development of a kit that utilizes enzymes to convert other blood types into the universal donor blood type O. The anchor then moved on to ask about the other applications of our project aside from resolving the blood shortage issue, in which we explained how our approach has potential applications in organ transplants and xeno transfusions. The interview audio clip can be found here.

Figure 33 - ICRT Logo
Education
7th Grade Education
In April, we hosted a seventh-grade event in which we taught TAS’ Class of 2026 basic synthetic biology concepts such as central dogma, gene sequence, and gel electrophoresis with a presentation and activities in order to introduce them to synthetic biology.
We began our presentation by giving the seventh graders a brief introduction to our project, which consisted of the dangers of transfusing incompatible blood types. By cutting off the ‘markers’, or antigens, that differentiate the different blood types, we can create universal O-type blood that can be transfused safely.
We continued by teaching the basics of synthetic biology, including central dogma and gene expression. With the topic of central dogma, we explained how DNA has to undergo transcription and translation to create proteins. With gene expression, we introduced the functions of the promoter, ribosome binding site, open reading frame, and terminator. We then switched to the topic of gel electrophoresis, which showed the seventh graders that parts of the DNA could be separated based on their sizes.
After our presentation, we started the experimental activities with the seventh graders, which consisted of a wet and dry lab part. For the wet lab, we taught them how to correctly use a pipette. With this knowledge, they were able to pipette 6 different colored charged dyes into the wells of agar gels, which we later ran so that the students could determine which dyes were positively or negatively charged. For the dry lab, we created various scenarios in which the students would have to assemble constructs from our cut-out gene sequences to solve the problem.

Figure 34 - An iGEM member teaching 7th graders Gel Electrophoresis

Figure 35 - 7th graders learning pipetting skills

Figure 36 - 7th graders listening to our presentation

Figure 37 - Presenting to 7th graders about our project
With this event, we were able to effectively engage with the seventh-grade students in these activities and successfully spark an interest in synthetic biology within them.

Figure 38 - Thank you card from 7th graders to iGEM team
Education Website
We launched our own educational website in early July of 2021 (tinyurl.com/TASTaipei-SynBioEducation) containing activity packets intended to teach those interested in learning about synthetic biology all over the world. This launch date coincides with summer break, providing resources for teachers who are preparing materials for the new school year or parents looking for summer learning material. Inclusivity is a central focus of this website; our free and downloadable activity packets come in both English and Mandarin Chinese, as does our website. We want to lower the barriers to education and allow everyone to have access to free learning resources to learn about fascinating science topics. These online activity packets are especially beneficial during the Covid-19 pandemic time period, as it allows students to learn safely without the need of in-person classes.
Each activity packet is composed of an instructional video, printable worksheet, and a “potential answer” answer key. To give an introduction to synthetic biology, there are 3 different activity packets: central dogma, gene expression, and gel electrophoresis. These downloadable materials allow people to learn scientific concepts without the need of lab materials. To make these materials applicable to younger ages, the worksheet activities are puzzle-based. When students complete an activity packet, they can email us a photo of their completed worksheet to receive a certificate.

Figure 39 - Home page of our Synthetic Biology educational website
We partnered with the BioBuilder Educational Foundation to create a Google Slide Presentation that digitized our “Gene Expression” activity packet. Educators can make their own copy of this presentation and make changes that will be adapted to their class. Along with BioBuilder, we distributed our education website to science-related Facebook groups as well as local schools.

Figure 40 - BioBuilder Educational Foundation’s logo
Educational Tiktoks
In May of 2021, we launched a Tiktok page to encourage exposure to synthetic biology through short informational videos. Our Tiktoks utilized helpful visual aids and analogies to provide easy-to-understand “crash courses” on a variety of topics. We produced videos with information on synthetic biology concepts, blood-related topics that connected to our project, fun scientific facts, as well as light-hearted trends that we adapted to involve the field of synthetic biology.

Figure 41 - TAS_Taipei’s Tik Tok Page
iGEM x Girls in Stem x FRC
In September of 2021, we partnered with Girls in STEM (GIS), a student organization within our school with a mission to mitigate the STEM gender gap, as well as our school’s First Robotics Competition (FRC) team to hold a collaboration event: STEM Workshop. STEM Workshop aimed to break down barriers students face when trying to enter STEM fields and allow students to gain an introductory understanding of the varying STEM fields. We invited young female students to explore, through hands-on experience, science, and technology fields. Our event promoted inclusivity and equity in male-dominated fields of study and encouraged young women to break down gender barriers in STEM. One survey found that out of 236 companies in the synthetic biology industry, only 14.4% (34 companies) were led by women (Hyde, 2018). However, synthetic biology, while still being a relatively new field, is able to fully address the gender inequality in STEM fields, and thus our workshop raised awareness while actively promoting female involvement in the field (Schyfter, 2020). TAS_Taipei, GIS, and FRC all held hour-long workshops in the fields of synthetic biology, data science, and robotics, respectively. TAS_Taipei’s own workshop focused on teaching and giving an introduction to DNA extraction and bacterial streaking.
The 30 participants, split off into three groups of ten, were first introduced to the field of Synthetic Biology and our team’s project. We then moved on to discuss the gender disparities that exist within the field and how TAS_Taipei is striving to reduce the stigmatization of women joining the STEM field. After that, we gave an introduction to the basics of DNA and went over each step of the protocol to extract DNA from strawberry samples. Participants then shifted to the hands-on portion of the workshop, where they followed the DNA extraction protocol with the help of our team members. After the DNA was successfully extracted from the strawberry cells, we regrouped and introduced the next activity, bacterial streaking. We first demonstrated how to streak agar plates, then allowed the participants to choose from a variety of colorful strains to draw on the plates with. Through this, the participants were able to learn lab techniques while having fun and creating art. We ended the workshop by explaining how bacterial streaking helps us with making proteins for our project and then sent the group of participants off to their next workshop as we waited for our next group to arrive.

Figure 42 - Participants extracting DNA from strawberries

Figure 43 - Bacteria designs created by STEM Workshop participants
Aboriginal School - TAS_Taipei X TAS IF Club X Jianshi Junior High School
In October of 2021, together with Initiative Formosa Club, another TAS organization promoting Taiwanese culture through service, we partnered with Jianshi Junior High School, a school serving the Atayal Aboriginal population of Jianshi Township, Hsinchu County, Taiwan. The Aboriginal population of Taiwan, having been historically discriminated against, now face a disadvantage in acquiring resources for education. With a mission to achieve equity in education, TAS_Taipei hosted a virtual introductory level lesson in science for students in 7th to 9th grade and sent over materials and equipment needed for the lesson.

Figure 44 - Virtual Lesson with Jianshi Jr. High Students
Our lesson first reviewed concepts of mass and volume, in turn giving an introduction to density, concentrations, and dilutions of solutions. The students were then introduced to lab equipment and techniques using the materials we sent over. After familiarising themselves with the lab skills, the students were given a colored solution and asked to conduct a serial dilution to a certain concentration, with a demonstration as an example. Then they were presented with a scenario involving diluting the solution until the color was no longer visible, and were asked to devise methods to calculate the concentration of the “clear” solution. Through this activity, we gave the students an increased opportunity to not only conduct hands-on experiments, but also to explore and help develop their interests in the sciences.

Figure 45 - Group photo with the Jianshi students
COLLABORATIONS
Through our collaborations, we not only received and sent help for our projects, we shared experiences, challenges and perspectives about synthetic biology and issues around our world.
iGEMxSDG Impact Challenge and Conference
As mentioned above in the "Sustainable Development" section, we hosted a global collaboration - iGEMxSDG Impact Challenge and Conference - among 26 teams across 16 countries. Learn more about the challenge above.
Participating iGEM Teams:
KCIS_NewTaipei, Korea_HS, NTU-Singapore, IISER-Tirupati_India, Saint_Joseph, RUBochum, Stony_Brook, CCU_Taiwan, SHSID, NKCU_Tainan, ASIJ_Tokyo, Moscow_City, Thessaly, Sydney_Australia, William_and_Mary, NU_Kazakhstan, Aachan, MIT_MAHE, PuiChing_Macau, Wageningen_UR, ATG X iGEM UMA, Open_Science_Global, Calgary, Tu_Darmstadt, Mingdao, TAS_Taipei
NYCU - Experimental Verification, Bacteria Strains, and Plate Reader Usage
We helped Team NYCU with one of their experiments by following the protocol they provided for us. Their experiment involved testing the effect of different promoter strengths on GFP expression after induction. We also provided them with E. coli Nissle 1917 Strains for them to use in their project. In return, they let us use their plate reader, which we used for our colorimetric enzyme functional tests.

Figure 52 - one of our members at NYCU running experiments

Figure 53 - Plate reader NYCU lended us to use for our enzyme functional experiments.
Patras Team - Comic Translations
Team Patras reached out to us for a collaboration for their pharmacogenomics project. They created a comic to help young children better understand how medicine and drugs work, and were seeking for teams to help translate the comic to different languages. Thus, we helped translate their comic into Mandarin, which can be found here. We hope that our translation will allow them to expand their audience and allow them to distribute their comic to global audiences.
Duesseldorf Team - Postcard Project
We participated in team Duesseldorf’s postcard project, a collaboration opportunity where teams design postcards about their project and send them to all other participating teams. Through this project, we were able to gain knowledge about the different projects from the 90 other participating teams. We hope that our postcard also enabled other teams to learn more about our project.

Figure 54 - Our postcard front cover design

Figure 55 - Our postcard back cover design

Figure 56 - Collection of all participating teams’ postcards
MingDao Team - Plasmid Constructs
Team MingDao reached out to us with a request for two plasmid constructs: T7 + RBS SplintR ligase Expressing Construct (BBa_K3352006) and " T7 + RBS Φ29 DNA polymerase Expressing Construct (BBa_K3352007). We gave these constructs to help their project and met up with them in a virtual conference call. In the conference, we learned about each other’s projects and exchanged public surveys, which both teams filled out and shared with other members of their community.
Korea_HS Team - Instagram Project
We participated in Korea_HS’s quarantine-themed Instagram project. This project aimed to create a sense of community during the pandemic. It allows teams to easily access contact/project information of other teams. We sent them our team photo and a 4~6 sentence description of our team and project.

Figure 57 - Instagram Post of our project’s information (image from Korea HS Instagram)
KCIS Team - Survey Distribution
We met up with the KCIS team in a virtual conference call. In the conference, we learned about each other’s projects and exchanged each other’s public surveys, which both teams filled out and shared with other members of each community. Their responses were used in our analysis of blood donation patterns around the world.
ARIA Team - Survey Distribution
The ARIA iGEM team helped distribute our public survey to members of their community. Their responses were used in our analysis of blood donation patterns around the world.
FURTHER APPLICATIONS
On top of addressing our project sustainability, we investigated additional applications and implementation of our project. From organ transplants to xenotransfusion, our project has wide-spread potential application.
Application on Organ Transplantation
Interview with Dr. Lori West on ABOi Organ Transplantation

Figure 58 - Interview with Dr. Lori West
During our interview with Dr. Lori West, a professor of Pediatrics and surgery at the University of Alberta, we explored the possibility of incorporating our project in the field of organ transplantation. Specifically, we hope to tackle ABO-incompatible transplantations, which hold relatively high risks and require many extra steps to ensure successful surgery, such as removing the recipient’s antibodies.
Through this interview, we learned more about the organ shortage that is present worldwide and the ever-increasing difficulty of obtaining an ABO-compatible organ transplant. We further learned about the various safety regulations that differ based on the country and some ethical considerations that we should be mindful of. Dr. West also expressed interest in our project and believes it is a great idea, but there are issues such as accommodation and antigen regeneration that should be considered. She emphasizes how more testing needs to be done to truly reveal the effect of our enzymes on the organs. Finally, she outlined a proposal for us to write up that encompasses literature research on why our project is important, why ABOi transplants do not occur currently, and the required experimentation on an animal model. Her inputs helped us in the development of a proposal for the application of our project to ABOi Transplants, which can be seen below.
Organ Transplantation Proposal
There is a perpetual shortage of organs globally. In the US alone, there are 107,000+ people on the waiting list for organ transplants as of February 2021, and a name is added to that list every 9 minutes (HRSA, 2021). In contrast, deceased donors provide on average 28,000 organs per year while living donors provide on average only around 6,000 organs per year (CDC, 2019). Combined with the layers of complexity of an organ donation system, the supply almost never meets the high demand. To make matters worse, according to Dr. Lori West, the onset of COVID has been detrimental to the supply of organs as programs for international donations have been shut down due to high restrictions. For those who are able to receive an organ transplant, they are often restricted to ABO-compatible organs to maximize graft survival rate, further limiting the availability of organs. In an attempt to ease the lopsided balance between supply and demand of organs, our team aims to use enzymes to cleave off the antigens on organs in order to achieve harmless ABO-incompatible organ transplants.
Although there have been discoveries to improve the efficiency and safety of ABO-incompatible transplants, they still rarely occur today. One of the reasons is the concern on blood group incompatibility, as antigens are present not only on the endothelial cells of the organ surface, but also on other important tissues. If the procedure fails to suppress the antibodies, they will latch onto the sugar group of the antigen and trigger a cascade of rapid destruction, or hyperacute rejection. When such a reaction occurs, clotting and thrombosis become inevitable and the organ is eventually destroyed (Lerman, 2018). Although methods such as plasmapheresis (a technique to separate blood antibodies from the blood serum), consumption of immunosuppressive drugs (suppresses the immunogenic reaction towards the foreign organ), and splenectomy (a technique that removes spleen, an abdominal organ that fights infection) are developed, there are still incredibly strict policies regarding ABOi transplants and few programs take on such high risk transplants (Salvadori and Tsalouchos, 2020).
Our enzymes, including endo-b-gal that removes A and B antigens, NAGA that removes A antigens, and a-Gal that removes B antigens, can theoretically remove the ABH antigens that are so prevalent on the various organs. Antigens were shown through immunofluorescence to be expressed on the hepatic artery, portal vein, capillary, sinusoidal lining cells, and liver epithelium in varying degrees (Rydberg, 2001). Through multiple ex vivo perfusions of the organs, which is the process in which a fluid is forced to continuously flow through the vessels of a biological tissue, we should be able to successfully cleave off the majority of the antigens of the organs (John Hopkins, 2021). We would then use immunohistochemistry, a method that uses antibodies to check for certain antigens in a tissue, to verify the effectiveness of our enzymes (National Cancer Institute, n.d.). However, different from blood-antigen removals, organ-antigen removals are not permanent as organs would still carry glycosyltransferases (enzymes responsible for the production of antigens). In fact, the antigenicity will recover within a few days. Even though the time window may seem short, this might just be all the patient needs to induce accommodation, or an absence of antigen-antibody reaction. When accommodation occurs, the organ survival rate greatly increases and the patient is avoided of hyperacute rejection. Since the greatest challenge with ABOi transplants is during the first few days after the transplant, the immune response during this time must be reduced for the success rate to greatly improve. Therefore, in order to instigate accommodation, blood antibodies should be suppressed to the lowest possible level during the first week post-transplant through the usage of immunosuppressive drugs (Kota Takahashi, 2005). Combined with the usage of our enzymes, the antigenicity would be extremely low at the start of the transplant and would, theoretically, induce accommodation reliably.
In the future, we would be looking to conduct experiments using animal organs to model that of humans. Past studies on pigs have shown that antigen expression can be reduced to an undetectable level through ex vivo perfusion of enzymes (Liu et al., 2002). However, considering the lack of research done about the utilization of enzymes to cleave organ antigens, more work also needs to be done on considering the regeneration of antibodies post-transplant and how that might affect accommodation, along with ethical considerations that require further discussions.
Application on Xenotransfusion
Besides our project’s application on ABOi organ transplantations, our project’s technology can also be applied to xenotransfusions. Xeno-transfusions are the transfer of blood from one species to another (non-human to human) (Roux et al., 2007). With blood shortages occurring globally due to lack in availability and compatibility, an alternative to human red blood cells will help increase the supply of blood as it does not depend on human blood donations (Smood et al., 2019). This procedure can further reduce risks of transmitting infectious diseases between humans and acna be done without affecting the health of the donor (Roux et al., 2007).
Studies have shown that porcine blood (pRBC) is the best candidate for xenotransfusions as it has more similar characteristics to human blood than other animals (Smood et al., 2019). For example, RBC size, typical RBC life span, RBC hemoglobin content, RBC structure, and other factors (Smood et al., 2019). A barrier that prevents xenotransfusion with porcine blood is that the antigens on pRBC cause immunological incompatibility between humans and pigs as human antibodies agglutinate with pRBC antigens. All porcine blood types have α-galactose (αGal) antigens present on their RBCs, and the αGal epitope is the major xenoantigen on pRBCs (Smood et al., 2019; Zhu, 2000). The αGal antigen has the same structure as the B antigen of human RBCs, with the only difference being the porcine antigen lacks a fucose sugar group (Fig. 59); thus, the porcien αGal reacts with human Anti-B antibodies, causing an immune response (Smood et al., 2019).

Figure 59 - Comparison of pRBC αGal antigen to human antigens. Shows that pRBC αGal structure is the same as human B antigen, except for the fucose group. (Smood et al., 2019)
Our enzyme conversion methodology can be applied to xenotransfusions to reduce immunological incompatibility. By using our α-galactosidase to enzymatically remove the aGal epitope on pRBC, human antibodies will no longer bind to pRBC antigens, and thus will not elicit an immune response. The α-galactosidase active site only binds to the terminal galactose, meaning the lack of fucose group does not affect the enzyme function on pRBC antigens (Guce, 2010). Past studies have shown that the αGal pRBC antigen was cleared by α-galactosidase and the structure and function of pRBC were normal (Smood et al., 2019). It also showed that in vitro binding of human antibodies to cleaved pRBC was greatly reduced (Smood et al., 2019). This provides evidence that our enzymatic conversion technology has potential to be applied to pRBC xenotransfusions, increasing the supply of blood for transfusions.
References
Roux, Françoise A.; Saï, Pierre; Deschamps, Jack-Yves (2007). "Xenotransfusions, past and present". Xenotransplantation. 14 (3): 208–216. doi:10.1111/j.1399-3089.2007.00404.x. ISSN 0908-665X. PMID 17489860.
Smood, Benjamin et al. “Genetically-engineered pigs as sources for clinical red blood cell transfusion: What pathobiological barriers need to be overcome?.” Blood reviews vol. 35 (2019): 7-17. doi:10.1016/j.blre.2019.01.003
Guce, Abigail Ida, "Structural and Mechanistic Studies of alpha-galactosidase A and Pharmacological
Chaperones" (2010). Open Access Dissertations. 202.
https://scholarworks.umass.edu/open_access_dissertations/202
Zhu A. Introduction to porcine red blood cells: implications for xenotransfusion. Semin Hematol. 2000 Apr;37(2):143-9. doi: 10.1016/s0037-1963(00)90039-8. PMID: 10791883.
“Organ Donation Statistics .” Health Resources & Services Administration, Oct. 2021, www.organdonor.gov/learn/organ-donation-statistics. Accessed 13 Oct. 2021.
Key Facts. 2021, www.cdc.gov/transplantsafety/overview/key-facts.html. Accessed 13 Oct. 2021.
Lerman, Mark. “ABO Incompatible Transplant Living Donor Education.” Youtube, uploaded by Medical City Dallas, 15 May 2018, https://www.youtube.com/watch?v=NeqmyJ_TK2U&t=172s.
Medical City Dallas. “ABO Incompatible Transplant Living Donor Education.” YouTube, 14 May 2018, www.youtube.com/watch?v=NeqmyJ_TK2U&t=172s. Accessed 13 Oct. 2021.
Salvadori, Maurizio, and Aris Tsalouchos. “Current Protocols and Outcomes of ABO-Incompatible Kidney Transplantation.” World Journal of Transplantation, vol. 10, no. 7, 29 July 2020, pp. 191–205, www.ncbi.nlm.nih.gov/pmc/articles/PMC7416363/, 10.5500/wjt.v10.i7.191. Accessed 13 Oct. 2021.
Takahashi, Kota. “A New Concept of Accommodation in ABO-Incompatible Kidney Transplantation.” Clinical Transplantation, vol. 19, no. s14, Aug. 2005, pp. 76–85, pubmed.ncbi.nlm.nih.gov/15955174/, 10.1111/j.1399-0012.2005.00392.x. Accessed 13 Oct. 2021.
“Ex Vivo Perfusion | Johns Hopkins Medicine.” Hopkinsmedicine.org, 20 May 2021, www.hopkinsmedicine.org/transplant/programs/Ex-Vivo-Perfusion.html. Accessed 13 Oct. 2021.
“NCI Dictionary of Cancer Terms.” National Cancer Institute, Cancer.gov, 2021, www.cancer.gov/publications/dictionaries/cancer-terms/def/immunohistochemistry. Accessed 17 Oct. 2021.
Rydberg, L. “ABO-Incompatibility in Solid Organ Transplantation.” Transfusion Medicine, vol. 11, no. 4, Aug. 2001, pp. 325–342, pubmed.ncbi.nlm.nih.gov/11532188/, 10.1046/j.1365-3148.2001.00313.x. Accessed 17 Oct. 2021.
Liu, DaGe, et al. “Enzymatic Removal of ΑGal Antigen in Pig Kidneys by Ex Vivo and in Vivo Administration of Endo-β-Galactosidase C.” Xenotransplantation, vol. 9, no. 3, 29 Apr. 2002, pp. 228–236, pubmed.ncbi.nlm.nih.gov/11983021/, 10.1034/j.1399-3089.2002.01068.x. Accessed 17 Oct. 2021.
Sustainable Development Goals. United Nations, sustainabledevelopment.un.org/
topics/sustainabledevelopmentgoals. Accessed 20 Oct. 2021.
THE 17 GOALS. United Nations, sdgs.un.org/goals.
“Voluntary Blood Donation: Foundation of a Safe and Sufficient Blood Supply.” Towards 100% Voluntary Blood Donation: A Global Framework for Action., U.S. National Library of Medicine, 1 Jan. 1970, www.ncbi.nlm.nih.gov/books/NBK305666/.
Chen, Emily Hui-Chen. “請不要再說捐血沒有成本,也不要再說我們是賣血的.” The News Lens 關鍵評論網, 14 Jan. 2017, https://www.thenewslens.com/article/59342.
Taiwan Blood Services Foundation. “TBSF 2019 Annual Report.” Taiwan Blood Services Foundation, 2019, http://intra.blood.org.tw/upload/6657d89b-a4e0-4311-a704-ec2fd0a4ff61.pdf.
衛生福利部中央健康保險署 . “總額支付制度意涵.” 衛生福利部中央健康保險署, 2005, https://www.nhi.gov.tw/Resource/webdata/32213_3_hosp_global_stable_eva_106y_1060112_ICD.ods.
Chen, Liang-fu. “健保給付「1點1元」,如何拯救台灣醫療?: 陳亮甫.” 鳴人堂, 鳴人堂 | 聯合新聞網, 9 Mar. 2020, https://opinion.udn.com/opinion/story/120803/4388788.
“Blood Types.” Explained - A, B, AB and O | Red Cross Blood Services, www.redcrossblood.org/donate-blood/blood-types.html.
“Demand for Different Blood Types.” NHS Blood Donation, www.blood.co.uk/why-give-blood/demand-for-different-blood-types/.
De Luca , G, et al. “Effects of Nickel on Human and Fish Red Blood Cells.” Bioscience Reports, U.S. National Library of Medicine, 27 Oct. 2007, https://pubmed.ncbi.nlm.nih.gov/17610155/.
Han, Yingchao, et al. “Nanosize and Surface Charge Effects of Hydroxyapatite ...” ACS, 3 Aug. 2012, https://pubs.acs.org/doi/10.1021/am300992x.
Tkeshelashvili, L. K., et al. “Effect of Some Nickel Compounds on Red Blood Cell Characteristics.” Biological Trace Element Research, Humana Press, 1989, https://link.springer.com/article/10.1007/BF02917273.
American Red Cross. “Winter Storms and Flu Prolong Blood Shortage.” American Red Cross, American Red Cross, 31 Jan. 2019, https://www.redcross.org/about-us/news-and-events/news/2019/winter-storms-and-flu-prolong-blood-shortage.html.
Chang, Yu-Wei, et al. “The Study of Anemia Prevalence in the Eastern Coastal Region of Taiwan.” Journal of Biomedical & Laboratory Sciences, Taiwan Society of Laboratory Medicine, 30 June 2016, https://www.airitilibrary.com/Publication/alDetailedMesh?docid=10137653-201606-201607110013-201607110013-63-69#.
Stermer, E, et al. “Seasonal Fluctuations in Acute Gastrointestinal Bleeding.” Journal of Clinical Gastroenterology, U.S. National Library of Medicine, June 1995, https://pubmed.ncbi.nlm.nih.gov/7665813/.
“8. The Chi Squared Tests | The BMJ.” The BMJ | The BMJ: Leading General Medical Journal. Research. Education. Comment, 28 Oct. 2020, https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/8-chi-squared-tests.
Yeager, Kristin. LibGuides: SPSS Tutorials: Chi-Square Test of Independence. https://libguides.library.kent.edu/SPSS/ChiSquare. Accessed 2 June 2021.
Larntz, Kinley. “Small-Sample Comparisons of Exact Levels for Chi-Squared Goodness-of-Fit Statistics.” Journal of the American Statistical Association, vol. 73, no. 362, [American Statistical Association, Taylor & Francis, Ltd.], 1978, pp. 253–63. JSTOR, doi:10.2307/2286650.
P Values (Calculated Probability) and Hypothesis Testing - StatsDirect. https://www.statsdirect.com/help/basics/p_values.htm. Accessed 2 June 2021.
“The Challenges of Treating Jehovah’s Witnesses.” n.d. Accessed October 21, 2021. https://www.medicalprotection.org/southafrica/casebook/casebook-may-2014/the-challenges-of-treating-jehovah%27s-witnesses.
“What Your Blood Type Says About You: A Fun, Educational Look at Your Health and Personality.” n.d. Accessed October 21, 2021. https://www.waldenu.edu/programs/health/resource/what-your-blood-type-says-about-you.
“Why Biotech Is Failing Women and How We Can Do Better - SynBioBeta.” n.d. Accessed October 21, 2021. https://synbiobeta.com/why-biotech-is-failing-women-and-how-we-can-do-better/.
“Gender in Synthetic Biology: Problems and Potential | EMBO Reports.” n.d. Accessed October 21, 2021. https://www.embopress.org/doi/full/10.15252/embr.201949049.

