Origin of our idea
After a lot of brainstorming and reflection we ended up choosing the “edible vaccine against SARS-CoV-2” as our project. Selecting a novel, smart and achievable project was not an easy task. It is a peculiar process that needs knowledge and experience but also young and curious minds to think of something new. As a team, at first, we needed time to bond with each other, eventually though we found our way and became a powerful team and friends in the process. Unfortunately, we were left behind schedule and we had to rush to find our perfect project for the iGEM competition. Therefore we started looking for new biological technologies as an inspiration. We worked hard to study a great deal of bibliography to decide if every idea we had was doable. After all that, we were presenting those same ideas to our P.I.s so we could receive their feedback and criticism on them. It was a time-consuming and stressful assignment especially under the pressure of time. In the end we found our final idea. Something fresh, smart, trending and above all something that can really help people, maybe even save some lives. It was a combination of things that helped us come up with this idea. We were very inspired by old iGEM projects, the technology we were looking at from the bibliography at the time, the teamwork and of course our P.I.s . They were always there to supervise, assist us, and indicate to us the right way.
Edible Vaccines
Advantages over Classical Vaccines
The coronavirus, a disease that arrived suddenly and progressed swiftly in just a few months, highlighted the importance of immunizations once more!
Conventional vaccinations have a number of drawbacks. The issue of safety is one of the most serious ones. Ιnjectable vaccinations can stimulate systemic humoral responses, although T cell effector function and mucosal immunity are critical for infectious disease prevention. Secondary effects of parenteral vaccination injection include local inflammation at the inoculation site, fever, and, in rare cases, hypersensitivity. Conventional approaches also make it impossible to generate vaccinations for all diseases. Due to these drawbacks, the idea of alternate vaccine delivery techniques emerged, paving the way for the creation of plant-based vaccines known as edible vaccines. Our team focused on developing edible vaccines as an alternative to injectable vaccinations in order to improve antigen stability and overall immunogenicity. New vaccine formulations that are edible or intradermal have been shown to elicit both a systemic and mucosal immune response. Oral vaccinations have a number of advantages versus injectable vaccines, including:

The production of edible vaccines
The manufacturing of edible vaccines is done by inserting a transgene into the selected plant cell. Transgene integration can be achieved either by vector (direct gene delivery) or without (indirect gene delivery). Gene delivery is facilitated by an Agrobacterium vector in order for plant cells to synthesize the desired protein in indirect gene delivery.
Agrobacterium is a gram-negative bacterium that affects plants by transferring its genes to the nucleus of the plant. Agrobacterium tumefaciens and Agrobacterium rhizogenes are the two most widely employed Agrobacterium species. The tumor-causing plasmid Ti is carried by Agrobacterium tumefaciens, while the root-inducing plasmid Ri is carried by Agrobacterium rhizogenes. This procedure is straightforward and cost-effective, but it is time-consuming and yields modest results.
When gene transfer via Agrobacterium is not possible, direct gene delivery involves inserting chosen DNA or RNA directly into the plant cell without the use of a vector, commonly by the biobalistic approach known as gene gun or microprojectile bombardment.
In our project, we picked Agrobacterium Tumefaciens for indirect gene administration since it is a current method of gene integration that is extensively utilized in transgenic plants while also being a simple and safe procedure of plant transformation. Agrobacterium transformation is also popular because it allows for the integration of well-defined DNA fragments, has a high rate of transgenic plant development, and is very inexpensive. Finally, most attempts to make edible vaccines, such as the cholera, Norwalk, and hepatitis B vaccines, used this strategy.
Exploiting the mucosal immunity
In addition to all of the advantages that edible vaccines give, they also provide critical protection by inducing both systemic and mucosal immunity, as opposed to standard vaccines that only elicit a mucosal response. The mucosal immune system is divided into two sections that work together. The mucosa-associated lymphoid tissues (MALTs) are inductive sites, which means that immune responses begin there. The effector locations, such as the lamina propria, are the second (LP). Immune responses and antibodies are produced in the effector sites. Our research is focused on the immunological response that Gut-associated lymphoid tissue (GALT) is in charge of.

Focusing on our topic, we will briefly discuss what happens when an immune response occurs following the ingestion of an antigen, in this case the spike S1 protein from SARS-CoV-2. M cells, which are found in the epithelial layer of the mucosal tissue and, more precisely, in the effector site (PPs), take the antigen and offer it to antigen-presenting cells (APCs), such as dendritic cells, at the beginning. M cells, more precisely, 'wake up' dendritic cells in the digestive system lumen, which now begin to transport the antigen (or peptides of it).
Finally, using chemokines, the processed peptides are delivered to naive T-cells, which begin to develop into antigen-specific cells such as Th1, Th2, Th17, and cytotoxic T cells.
The B-cells that have now matured into IgA-B cells migrate from the inductive site (PPs) through the lymph vessels to the lymph nodes and the effector site once the immune response has been initiated (LP). Finally, the Th2-type cytokines lead IgA-B cells to develop into plasma cells (IL-5 and IL-6). The interaction of IgA with the polymeric Ig receptor results in the production of secretory IgA. (SIgA).
The mucosal surfaces of the gut intestines are important routes of entry into the body for the majority of infections due to their large surface area. As a result, novel vaccinations, like the one we propose, are very desirable. Mucosal immunization with an appropriate vaccine delivery method induces both protective mucosal and systemic immune responses, resulting in a second layer of pathogen protection. However, only a low number of mucosal vaccines has been produced and used against human diseases. This is owing to obstacles such as determining the best vaccine formulation, including the adjuvant, to enhance immunogenicity, stability, and delivery. We want to contribute to such a vaccination development through our project: 'vaccinATEd.'
Project Idea
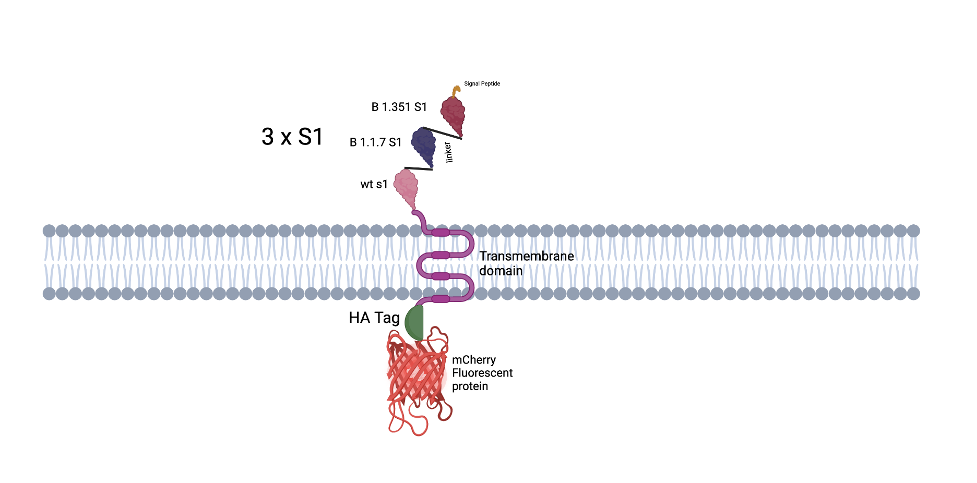
Agrobacterium tumefaciens cells, transformed with a plasmid construct expressing the antigen, will be introduced into Lactuca sativa (lettuce) leaves for transient expression of the synthetic protein. The synthetic protein consists of a signal peptide (SP), three copies of the S1 subunit of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) connected with an amino acid linker, a transmembrane (TM) domain, an HA (Human influenza hemagglutinin) tag and a fluorescent protein (mCherry).